Teenage Gynecomastia











For many adolescent boys, the physical changes of puberty are challenging enough—but the unexpected development of breast tissue can be especially difficult to cope with.
Teenage gynecomastia, also known as pubertal gynecomastia, refers to the benign enlargement of male breast tissue that commonly appears during early puberty. While it often resolves on its own, persistent breast enlargement that lasts beyond one to two years may require clinical assessment and potentially surgical treatment.
At our Newport Beach practice, Dr. Joseph T. Cruise specializes in treating gynecomastia in adolescent males. With over 5,000 gynecomastia surgeries performed, he offers unmatched experience in diagnosing and correcting all types of male breast tissue development. His approach focuses on accuracy, transparency, and delivering results that are both natural-looking and psychologically impactful.
Teen gynecomastia occurs when hormonal changes trigger the proliferation of male breast tissue, often seen as puffy nipples, palpable breast tissue, or moderate breast enlargement. This may affect one or both breasts and often causes psychological distress or significant embarrassment during a critical time of identity development. While physiologic gynecomastia is common among adolescent boys, persistent gynecomastia—especially with dense breast tissue or pain or tenderness—may need to be evaluated.
Factors such as elevated female hormone levels, the activity of the aromatase enzyme complex, or abnormalities in the pituitary glands can contribute to sustained breast development. In rare cases, secondary conditions like Klinefelter syndrome, testicular tumors, or congenital adrenal hyperplasia may be involved and should be ruled out through a comprehensive medical history and physical examination.
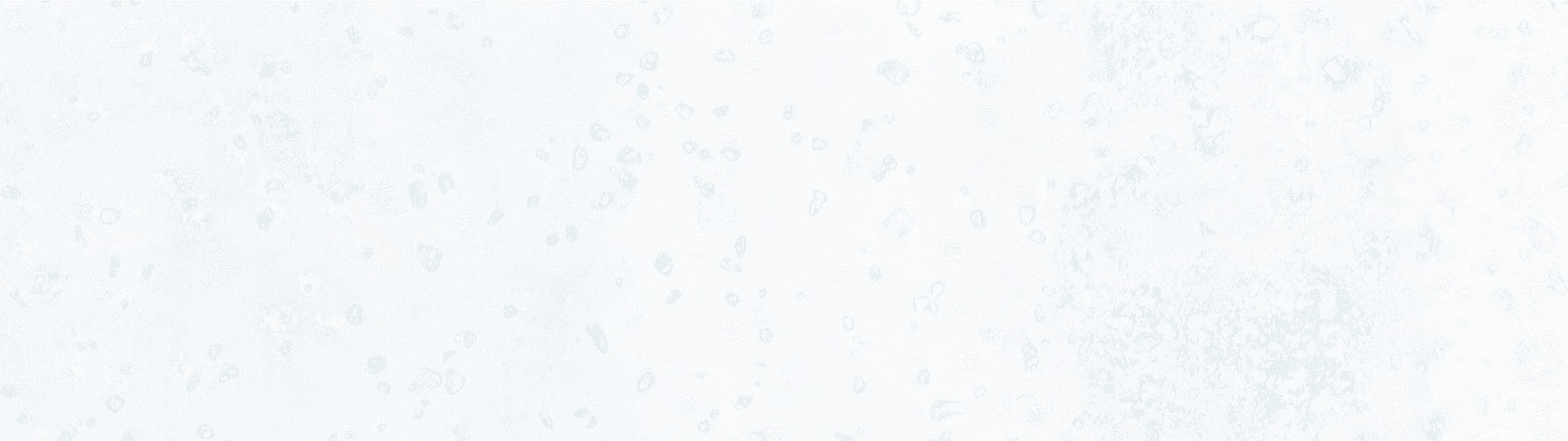
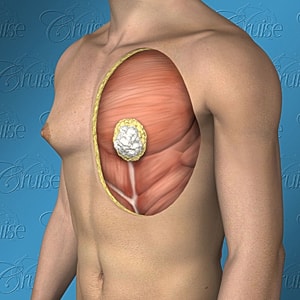
Dr. Joseph T. Cruise has performed over 2,500 gynecomastia surgeries, giving him the experience needed to recognize that not all cases are the same. Through this expertise, he developed the Cruise Classification System—a structured approach that identifies six distinct types of gynecomastia. Each type has its own characteristics and requires a tailored surgical strategy to achieve the best outcome. Dr. Cruise determines the most appropriate treatment by:
By using this system, Dr. Cruise is able to consistently deliver results that are not only natural-looking, but also aligned with the individual needs of each patient.

Notice the progressive increase in skin laxity. This excess skin will change the type of surgery necessary to properly correct the problem.






Type 1 gynecomastia, often known as puffy nipples, is the mildest form of the condition. In these cases, the excess tissue is located primarily beneath the nipple and areola, with little to no spread across the rest of the chest.
Because the surrounding skin remains firm and tight, it wraps cleanly around the pectoral border, maintaining a more defined and straight chest contour. Unlike more advanced types, Type 1 does not involve significant fat or glandular tissue extending beyond the nipple area. This is what differentiates it from Type 2 gynecomastia, where the tissue pushes past the pectoral edge, often leading to a rounder, less defined chest fold. Some individuals with Type 1 may also notice mild tenderness in the area, a common symptom when glandular tissue is present beneath the surface.

Characterized by puffy nipples. Patients are typically young, thin with a straight, well-defined pectoralis muscle
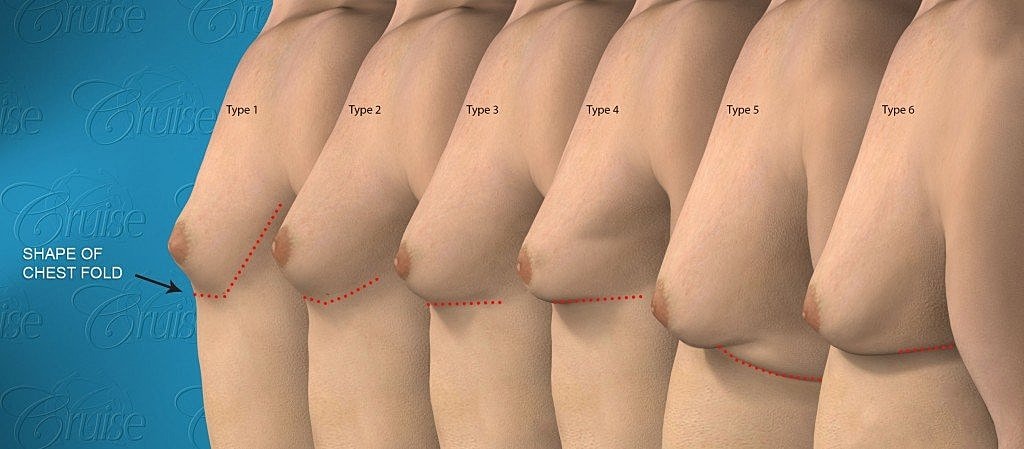
Notice the firm, white, breast glands located almost exclusively underneath the nipple/areola. This excess fatty tissue is what creates puffy nipples.
Type 1 gynecomastia is commonly identified by puffy nipples—a condition most often seen in younger, leaner patients with otherwise well-defined pectoral muscles. From the outside, the chest appears fit, but the nipple area protrudes slightly due to tissue buildup beneath the surface.
In these cases, the excess tissue is made up primarily of dense, white glandular material located directly under the nipple and areola. This concentrated buildup is what causes the puffy appearance, even in patients with low body fat and strong muscle tone.
Although it’s considered the mildest form of gynecomastia, Type 1 is not always the easiest to treat. Because these patients are often in excellent physical condition, even subtle imperfections—like residual puffiness, contour irregularities, or cratering—can stand out. Patients with puffy nipples typically have high expectations, and rightfully so.
Achieving the best possible outcome requires more than simply removing tissue. It takes a thoughtful, detail-oriented approach that anticipates and prevents potential complications. Unfortunately, gynecomastia has historically received less attention than other aesthetic procedures in the surgical community. That’s why platforms like this exist—to share insight, elevate the standard of care, and guide patients and surgeons toward consistently better outcomes.

External view of masculine chest
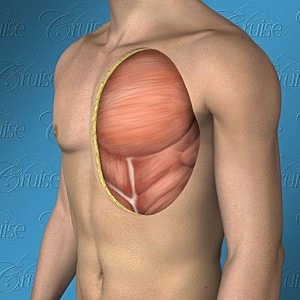
Internal view of masculine chest
Gynecomastia surgery is an outpatient procedure performed under general anesthesia that typically takes 1 to 2 hours.
Incision placement will depend on the patient’s individual anatomy. Dr. Cruise places the incisions in natural creases, or along the border of the areola, to minimize visible scarring. Glandular tissue is excised, and liposuction may be used to remove any excess fat, if present. The incisions are then closed using precise techniques to promote smooth healing. After a short monitoring period, the patient returns home the same day with an aftercare plan in place.
For patients with mild Type 1 gynecomastia, visible scarring is rarely a concern. Because the skin is tight and the excess tissue is localized beneath the areola, incisions can typically be placed within the natural border of the nipple. Even in cases that require a more advanced approach, such as the superior crescent incision, the scar remains discreet thanks to the natural transition in texture and color between areolar and chest skin.
Balancing Minimal Scarring With Ideal Chest Shape
Most Type 1 patients won’t need large incisions, since their skin quality supports a clean contour without extra tightening. When needed, a small incision around the areola is usually enough to access and remove the gland. However, in some individuals with naturally low-set nipples, the surgeon may need to adjust the position slightly to keep the nipple centered along the chest wall. Without this adjustment, the nipple can sit too low post-surgery, creating a “cratered” or sunken appearance along the pec border. This scenario may call for a superior areola incision—still subtle, but slightly more visible.
An inferior crescent excision involves removing a narrow, crescent-shaped piece of skin just below the areola.
While small, this adjustment can significantly enhance chest definition. It tightens the surrounding skin and smooths out any mild laxity, similar to flattening a wrinkle in a sheet. The incision sits along the lower edge of the areola, making it difficult to detect, even in early healing stages.
One thing to note with crescent incisions: the curved edges of the skin don’t always match perfectly when rejoined. This can cause minor bunching in the early healing phase, but it typically smooths out as the tissue settles and scars mature.

Along with aesthetic conditions, gynecomastia carries an emotional burden that is both profound and often misunderstood. While some men—typically older—may cope with minimal psychological impact, younger individuals, especially teens, can experience deep distress. For them, the condition can quietly affect self-esteem, social interactions, and mental health to a degree that is rarely acknowledged in traditional medical settings.
Because gynecomastia is tied to physical development during a critical stage of identity formation, its effects often go far beyond the chest. Teens may feel isolated, believing they’re the only ones dealing with it. Many are unaware the condition even has a name. Others may feel too ashamed to speak to family or friends. As a result, they often retreat inward, turning to the internet in search of answers or support—making them easy targets for misinformation, unproven “miracle” products, or worse, emotional manipulation from bad actors.

The emotional toll of living with gynecomastia during adolescence can manifest in subtle or overt ways. Teens may seem withdrawn or avoid activities they once enjoyed. Even everyday situations—like gym class or being invited to the beach—can feel like sources of dread. Many report:
This isn’t just about body image—it’s about identity, confidence, and the quiet psychological strain that can shape a young person’s life if left unaddressed. Recognizing these signs is often the first step in helping someone find the care and support they need.
“It feels embarrassing having a femininely shaped chest. I didn’t feel masculine and it caused me great anguish. Usually I avoided situations that required me to take my shirt off, like swimming. I would hunch my shoulders so that my shirt would drape over my chest, because I was afraid other people would notice my chest. A friend of mine told me I had man-boobs and I immediately realized that other people noticed what I had seen all along. I immediately felt embarrassed and wanted to disappear. Normally I would wear loose fitting shirts and hunch my shoulders so that my chest wouldn’t protrude. I was unable to stick my chest out with pride (literally). Try diet and exercise to see if you can reduce the appearance of your gynecomastia. If you’re still unhappy, research a competent surgeon. That’s the route I took and I was fortunate enough to find Dr. Cruise.
I did pursue gynecomastia surgery and the only regret I have is that I did not do it sooner. I’m so pleased with the results that I can not wait for the summer so I can walk along the beach with my shirt off. The boost to my confidence has been enormous. I totally believe it was worth it. The biggest impact I’ve seen (besides my confidence) is that I’m able to stand up straight again without worry about my “man-boobs” protruding. Something as simple as standing up straight not only makes me look more confident, but I feel more confident. “
Gynecomastia in teens often goes unspoken—but the signs are there if you know what to look for. As a parent, you may notice subtle shifts in your son’s behavior that suggest he’s uncomfortable with his body, even if he hasn’t said anything directly.
Is he avoiding shirtless activities he once enjoyed, like swimming or sports? Does he insist on wearing a shirt at the beach or opt for oversized clothing that hangs away from the chest? Has he become more withdrawn, negative, or made excuses to skip PE? In some cases, teasing or comments from peers—whether playful or cruel—can make a sensitive issue even harder to talk about.
Many teens don’t realize their condition has a name, and most won’t bring it up on their own. Creating a safe space for conversation is the first step. Choose a quiet, private moment to gently ask about what you’ve observed. If you can reference a specific event, like skipping a pool party or always layering clothing, it helps make the conversation feel grounded and caring rather than confrontational.
“I noticed you didn’t go swimming last weekend with your friends, and I know how much you usually enjoy that. I just wanted to check in—are you feeling okay?”
“You’ve seemed hesitant to join activities that involve taking your shirt off. If something about your body is bothering you, I want you to know you can talk to me about it, no judgment.”
You can also introduce educational material—like an article or video—so your teen doesn’t feel pressured to explain everything on the spot. Keep in mind: the goal is to let your son know you’re there for him, you’re open to listening, and most importantly, you’re not there to judge.
Gynecomastia surgery offers lasting relief from both physical symptoms and the emotional burden of breast enlargement. Most patients report a dramatic improvement in confidence, posture, and overall well-being.
Benefits include:
When performed by an experienced surgeon, surgical correction of teenage gynecomastia can be life-changing.
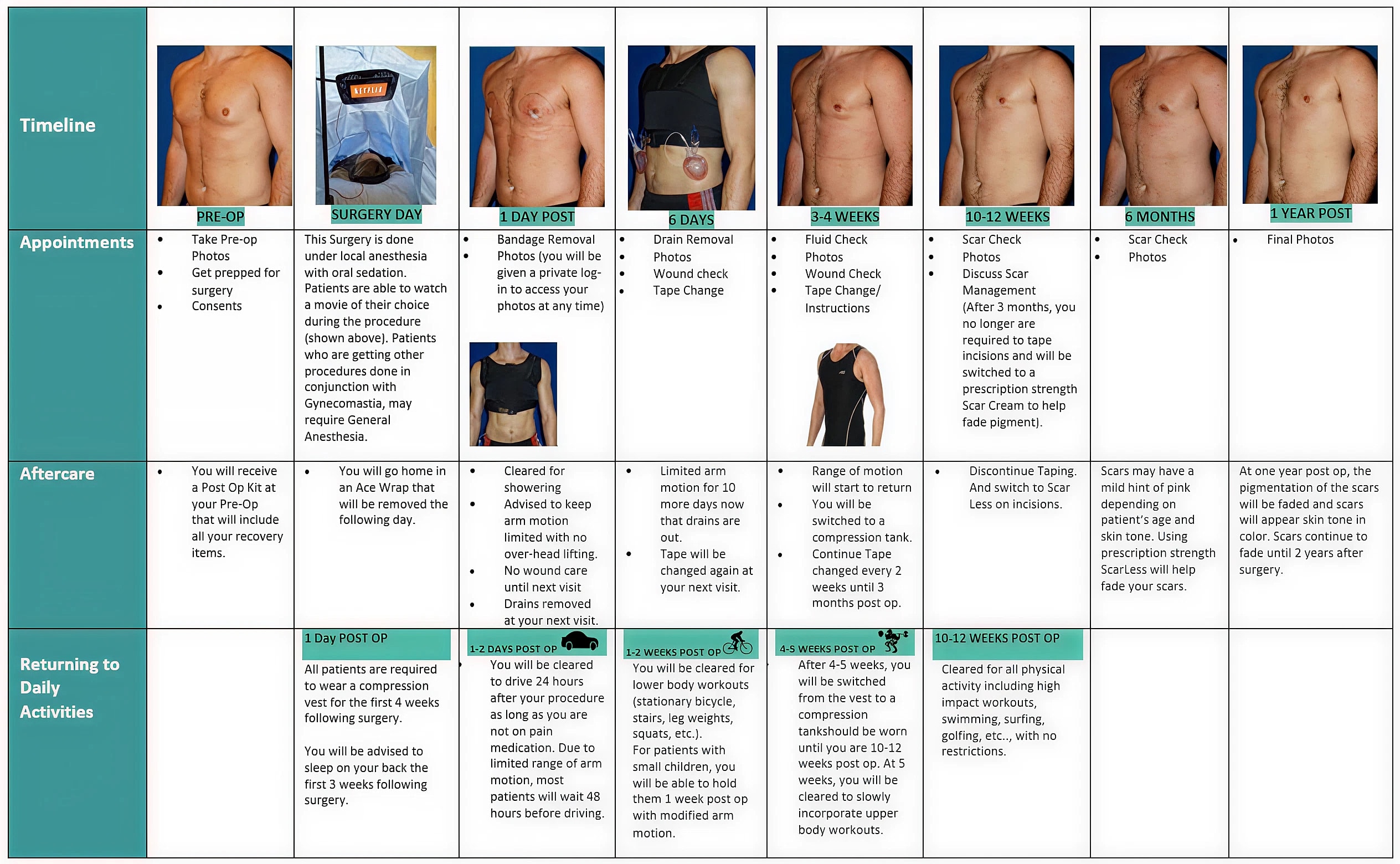
Gynecomastia surgery results in a flatter, more defined chest that better matches the patient’s frame and physical development. Results are permanent, as long as hormonal levels are stable and no new underlying conditions develop. For many young men, this leads to improved self-confidence, freedom in clothing choices, and a more positive relationship with their body.
While the physical change is important, the emotional impact is often even greater. Surgery can help teens move forward without the burden of self-consciousness that can define their school years.


Explore our before and after photo gallery to see real results from Type 1 gynecomastia (puffy nipple) surgery. Keep in mind that every patient’s body is different, and outcomes may vary based on individual anatomy and treatment approach.
1 of 3
Dr. Joseph T. Cruise is one of the few surgeons in the U.S. who has made gynecomastia a central part of his practice.
With more than 70% of his patients being male, he brings not only surgical expertise but a deep understanding of how this condition affects young men physically and emotionally. Parents appreciate his honest, no-pressure approach. Teens appreciate that he listens. If surgery is not the right step, he’ll tell you. If it is, you can be confident it will be done with care, precision, and long-term results in mind.

With over 5,000 gynecomastia procedures performed, Dr. Cruise brings an exceptional level of experience and precision to every case. To get started, schedule a consultation by completing our online form or calling our office at 949-644-4808.
Very common. Up to 70% of teenage boys experience some form of gynecomastia during puberty. For many, it resolves on its own, but for others, it may become permanent.
Surgery is typically considered for teens over 15 who have had stable gynecomastia for at least a year and whose bodies are mostly developed.
Most procedures take 1 to 2 hours and are performed as outpatient surgeries under general anesthesia.
Incisions are small and placed strategically, usually along the edge of the areola. Scars typically fade over time and are minimally visible.
As long as hormone levels remain stable and there’s no underlying cause like anabolic steroids or testicular masses, results are typically permanent. Long-term satisfaction is high, especially when realistic expectations are established during the consultation process.
Most teens return to school within a few days, though physical activities like sports will need to be paused for a few weeks.
Yes, when performed by an experienced, board-certified plastic surgeon. Dr. Cruise has treated many teenage patients with excellent outcomes.